
By Matthew Celentano
The writer is executive director of the League of Life & Health Insurers of Maryland, Inc., the state trade association representing the life and health insurance industry.
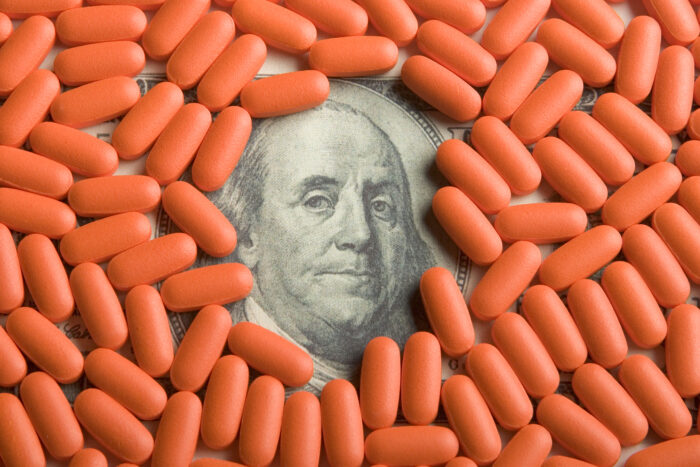
Prescription drugs and their astronomical costs have been a frequent topic of debate during the 2024 Maryland General Assembly Session.
The high list prices set by the drug manufacturers — prices set without any justification or regulation — have an incredible impact on insurance design and insurance premiums. High costs continue to squeeze consumers in a fashion that makes life-saving drugs unaffordable.
About a decade ago, prescription drugs accounted for less than 10% of your insurance premium. Because of unjustifiable drug price increases by the manufacturers, that percentage has skyrocketed to over one-third of premiums today.
That is why when Senate Bill 595/House Bill 879 was introduced, health insurers were concerned about the negative impact it would have on costs. While on its face, the bill appears to be a no-brainer by allowing discounts provided in the form of a coupon by a manufacturer to count towards a deductible, there is more to the story.
We know drug manufacturer coupons create additional insurance premium spending while netting windfall profits for manufacturers. The federal government has labeled the schemes in the bill as introduced as “kickbacks” for manufacturers and has historically not honored them in federal programs. These are the reasons insurers were concerned with the bill as introduced. Still, through conversations and the leadership of Del. Steve Johnson (D-Harford), amendments that mitigated insurers’ concerns and protected consumers were adopted in the House.
This week in Maryland Matters, the Immune Deficiency Foundation (IDF) highlighted legislation passed in the District of Columbia, which is substantially similar to SB 595/HB 879 as amended. They referenced that 19 other states passed this bill, however, they neglected to mention that more than a majority of those states mirror the amended SB 595/HB 879. The amendments include language addressing generic alternatives and health savings accounts (HSA) and high deductible health plans. The HSA language is written identically to Maryland HSA exemption language used throughout the Code, at the request of the Maryland Insurance Administration, the primary insurance regulator in the state.
To further empower consumers, the House also added a provision mandating that drug manufacturers communicate with patients about what to expect with a coupon and when the discount will disappear. Providing consumers with information should be seen as empowering and transparent, yet IDF confusingly opposes this provision.
What is also baffling is that IDF was present during the early legislative discussions where carriers suggested the aforementioned amendments and never objected to the proposals. Two weeks passed between that meeting and the bill hearing and concerns were not raised with the House sponsor at any point.
The stakeholders left the meeting thinking a compromise had been reached. Now, IDF is publicly working against the bill and the benefits to consumers it represents.
While coupons can result in savings for a subset of patients, the real financial benefit goes to drug makers who get to keep supplying the patient with their high-cost product. These dollars never go to plans or the benefit companies they use to manage pharmacy benefits.
The assertion that health plans and their pharmacy benefits managers (PBMs) are receiving funds when coupons are used is simply not true. League carriers take issue with IDF’s repeated narrative that PBMs are receiving copay assistance money. Like any other coupon, these coupons are managed at the place of purchase (the pharmacy), not by the PBM.
The simplest, most effective way to reduce patient costs for health care is for manufacturers to drop the price of the drugs. Until then, HB 879 can help increase transparency in drug prices and reduce the bait-and-switch tactics that plague our healthcare system. It strikes a balance of helping consumers with their out-of-pocket costs while ensuring that manufacturers cannot continue their opaque strategies of marginalizing regulated health care entities while increasing costs for all Marylanders.


 Creative Commons Attribution
Creative Commons Attribution